Implementing Shared Decision Making in Clinical Practice
Learn more about the development process and the key aspects of SDM:HOSP - a generic model for hospital-based implementation of shared decision making.
Shared Decision Making is a fundamental aspect of the interaction between patients and healthcare professionals. However, integrating shared decision making into routine clinical practice has proven challenging.
In an effort to create lasting change, the Region of Southern Denmark set out to develop a sustainable model for implementing shared decision making. The approach is grounded on insights and lessons learned from large-scale, real-world implementation efforts across several hospitals in the Region. Rather than focusing solely on identifying barriers and facilitators, the work aimed to understand what it takes to integrate Shared Decision Making into routine clinical practice.
The outcome of this work is SDM:HOSP—a generic implementation model designed to embed shared decision making into everyday clinical workflows. This page presents the key components of the model.
Read more about the SDM:HOSP development process in the publication:
SDM:HOSP - Our model for implementation of shared decision making
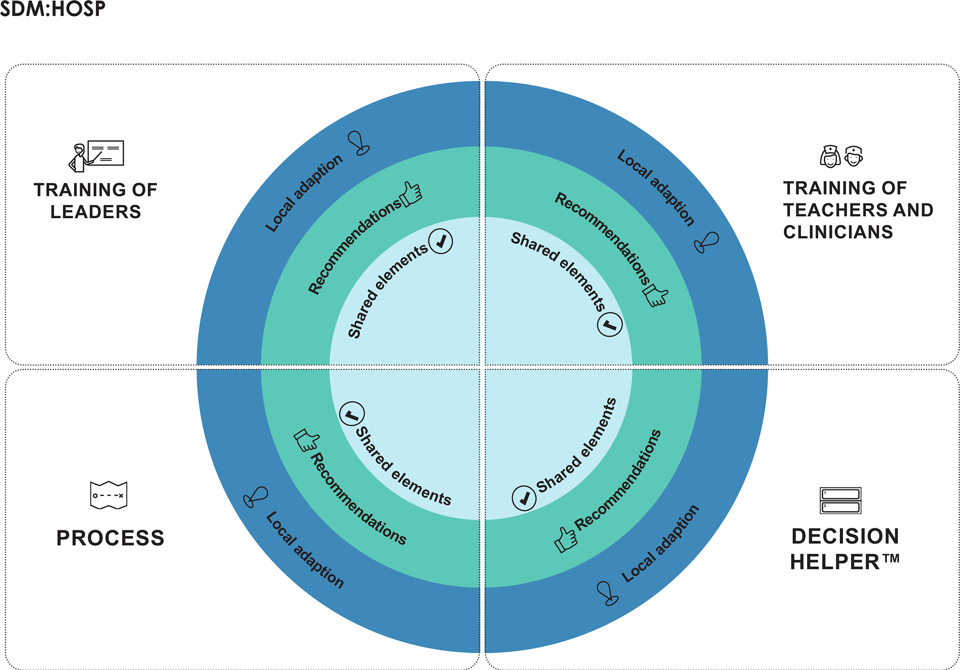
The SDM:HOSP model is designed to support the sustainable implementation of shared decision making in clinical practice. It is structured around four core components, each containing shared elements, recommended elements and elements that can be locally adapted.
To explore the model in more detail, you can expand each component below to see its key elements and guidance for implementation.
Shared elements:
- Organise a course of min. three hours in shared decision making for leaders
- Teachers are local implementation consultants with feedback from teachers of Center for Shared Decision Making
- Obligatory course material
Recommendations:
- Leaders at all levels participate in the course
- As many leaders as possible from the same department* participate over time
Local adaption of elements:
- Local supplements to obligatory course material
- Center for Shared Decision Making can be involved in case of large classes
*Definition of department depends on the setting. It may also refer to a section, a team or a clinical field.
Shared elements:
- Two-days teach-the-teachers courses, facilitated by teachers from the Center of Shared Decision
Making and local implementation consultants - Courses in shared decision making for clinicians, facilitated by educated local teachers
- Obligatory course material for both courses
Recommendations:
- Teachers from several professions are trained with emphasis on doctors
- At least two teachers are trained in small teams/sections, and at least four teachers in large departments/sections
- Once trained, the teachers must have time to plan and perform courses
- Teachers should have contributory influence on local implementation
Local adaption of elements:
- Defining the role of the teachers in addition to teaching
- Preparing teachers for pre-defined role
- Duration of courses in shared decision making for clinicians
- Number of participants in courses in shared decision making for clinicians
- Use of e-learning tools
Shared elements:
- Development of at least one DECISION HELPER™** per department*
- Patient involvement is obligatory when developing the DECISION HELPER™
Recommendations:
- Organise workshops when developing the DECISION HELPER™
- Local focus on the quality of the Decision Helpers designed, in addition to the International Patient Decision Aids Standards criteria
Local adaption of elements:
- Use methods from the Health Care Improvement Model in the Region of Southern Denmark in the development process
* Definition of department depends on the setting. It may also refer to a section, a team or a clinical field
** In the Region of Southern Denmark, the DECISION HELPER™ is applied by default. In exceptional cases, other generally approved patient decision aids can be used if agreed by the hospital management. The aid must fulfil the International Patient Decision Aids Standards criteria.
Shared elements:
- Preparatory meetings with clinical leader teams as kick-off for implementation
- A systematic process and sustainability plan is prepared and integrated into the process, entailing a fixed series of meetings and standard agenda
Recommendations:
- Patients should be engaged in the implementation activities in the department*
- Use materials that activate the patients during the decision process
- Initiate implementation activities focusing on the department’s culture of involving patients
- Use methods already know from the Health Care Improvement Model in the Region of Southern Denmark
Local adaption of elements:
- Number of departments* working on implementation
- Duration of the process and sustainability plan
- Content on the standard agenda
- Implementation activities in clinical departments*
- Random checks of OPTION12 measurements as an indicator for progress in the department* and for feedback, both individually and in groups
*Definition of department depends on the setting. It may also refer to a section, a team or a clinical field.